The Role and Function of the Spinal Cord and Spinal Nerves in Transmitting Sensory and Motor Information Throughout the Body,
The Spinal Cord and Spinal Nerves and Homeostasis
About 100 million neurons and even more neuroglia compose the
spinal cord, the part of the central nervous system that extends
from the brain. The spinal cord and its associated spinal nerves
contain neural circuits that control some of your most rapid
reactions to environmental changes. If you pick up something hot,
the grasping muscles may relax and you may drop the hot object
even before you are consciously aware of the extreme heat or
pain. This is an example of a spinal cord reflex—a quick, automatic
response to certain kinds of stimuli that involves neurons only in
the spinal nerves and spinal cord. Besides processing reflexes,
the gray matter of the spinal cord also is a site for integration
(summing) of excitatory postsynaptic potentials (EPSPs) and
inhibitory postsynaptic potentials (IPSPs), which you learned about
in Chapter 12. These graded potentials arise as neurotransmitter
molecules interact with their receptors at synapses in the spinal
cord. The white matter of the spinal cord contains a dozen major
sensory and motor tracts, which function as the “highways” along
which sensory input travels to the brain and motor output travels
from the brain to skeletal muscles and other effectors. Recall that
the spinal cord is continuous with the brain and that together they
make up the central nervous system (CNS).
Q Did you ever wonder why spinal cord injuries can have
such widespread effects on the body?,
Spinal Cord Anatomy
OBJECTIVES
• Describe the protective structures and the gross anatomical
features of the spinal cord.
• Explain how spinal nerves are connected to the spinal cord.
Protective Structures
,
Recall from the previous chapter that the nervous tissue of the central
nervous system is very delicate and does not respond well to injury or
damage. Accordingly, nervous tissue requires considerable protec-
tion. The first layer of protection for the central nervous system is the
hard bony skull and vertebral column. The skull encases the brain and
the vertebral column surrounds the spinal cord, providing strong pro-
tective defenses against damaging blows or bumps. The second pro-
tective layer is the meninges, three membranes that lie between the
bony encasement and the nervous tissue in both the brain and spinal
cord. Finally, a space between two of the meningeal membranes con-
tains cerebrospinal fluid, a buoyant liquid that suspends the central
nervous tissue in a weightless environment while surrounding it with
a shock-absorbing, hydraulic cushion.
Vertebral Column The spinal cord is located within the vertebral
canal of the vertebral column. As you learned in Chapter 7, the vertebral
foramina of all of the vertebrae, stacked one on top of the other, form the
vertebral canal. The surrounding vertebrae provide a sturdy shelter for
the enclosed spinal cord (see Figure 13.1b). The vertebral ligaments,
meninges, and cerebrospinal fluid provide additional protection.
Meninges The meninges (me-NIN-jēz; singular is meninx [ME-
–
ninks]) are three protective, connective tissue coverings that encircle
the spinal cord and brain. From superficial to deep they are the
(1) dura mater, (2) arachnoid mater, and (3) pia mater. The spinal
meninges surround the spinal cord (Figure 13.1a) and are continu-
ous with the cranial meninges, which encircle the brain (shown in
Figure 14.2a). All three spinal meninges cover the spinal nerves up
to the point where they exit the spinal column through the interver-
tebral foramina. The spinal cord is also protected by a cushion of fat
and connective tissue located in the epidural space (ep′-i-DOO-ral),
a space between the dura mater and the wall of the vertebral canal
(Figure 13.1b). Following is a description of each meningeal layer.
1. Dura mater (DOO-ra MĀ-ter = tough mother). The most superficial
of the three spinal meninges is a thick strong layer composed of
dense irregular connective tissue. The dura mater forms a sac from
the level of the foramen magnum in the occipital bone, where it is
continuous with the meningeal dura mater of the brain, to the
second sacral vertebra. The dura mater is also continuous with the
epineurium, the outer covering of spinal and cranial nerves.
2. Arachnoid mater (a-RAK-noyd MĀ-ter; arachn- = spider; -oid =
similar to). This layer, the middle of the meningeal membranes, is
a thin, avascular covering comprised of cells and thin, loosely ar-
ranged collagen and elastic fibers. It is called the arachnoid mater
because of its spider’s web arrangement of delicate collagen fibers
and some elastic fibers. It is deep to the dura mater and is continu-
ous through the foramen magnum with the arachnoid mater of the
brain. Between the dura mater and the arachnoid mater is a thin
subdural space, which contains interstitial fluid.
3. Pia mater (PĒ-a MĀ-ter; pia = delicate). This innermost meninx is a
thin transparent connective tissue layer that adheres to the surface
of the spinal cord and brain. It consists of thin squamous to cuboidal
cells within interlacing bundles of collagen fibers and some fine
elastic fibers. Within the pia mater are many blood vessels that
supply oxygen and nutrients to the spinal cord. Triangular-shaped
membranous extensions of the pia mater suspend the spinal
cord in the middle of its dural sheath. These extensions, called
denticulate ligaments (den-TIK-ū-lāt = small tooth), are thicken-
ings of the pia mater. They project laterally and fuse with the arach-
noid mater and inner surface of the dura mater between the anteri-
or and posterior nerve roots of spinal nerves on either side (Figure
13.1a, b). Extending along the entire length of the spinal cord, the
denticulate ligaments protect the spinal cord against sudden dis-
placement that could result in shock. Between the arachnoid mater
and pia mater is a space, the subarachnoid space, which contains
shock-absorbing cerebrospinal fluid.
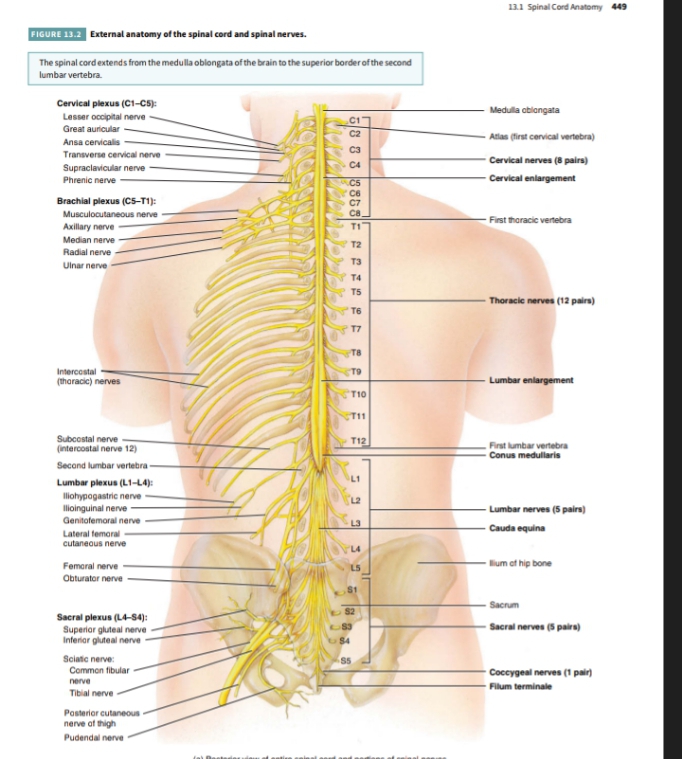
External Anatomy of the Spinal Cord
،
The spinal cord is roughly oval in shape, being flattened slightly ante-
riorly and posteriorly. In adults, it extends from the medulla oblon-
gata, the inferior part of the brain, to the superior border of the second
lumbar vertebra (Figure 13.2). In newborn infants, it extends to the
Q What are the superior and inferior boundaries of the spinal dura mater?
third or fourth lumbar vertebra. During early childhood, both the spi-
nal cord and the vertebral column grow longer as part of overall body
growth. Elongation of the spinal cord stops around age 4 or 5, but
growth of the vertebral column continues. Thus, the spinal cord does
not extend the entire length of the adult vertebral column. The length
of the adult spinal cord ranges from 42 to 45 cm (16–18 in.). Its maxi-
mum diameter is approximately 1.5 cm (0.6 in.) in the lower cervical
region and is smaller in the thoracic region and at its inferior tip.
When the spinal cord is viewed externally, two conspicuous
enlargements can be seen. The superior enlargement, the cervical
enlargement, extends from the fourth cervical vertebra (C4) to the
first thoracic vertebra (T1). Nerves to and from the upper limbs arise
from the cervical enlargement. The inferior enlargement, called the
lumbar enlargement, extends from the ninth to the twelft h thoracic
vertebra. Nerves to and from the lower limbs arise from the lumbar
enlargement.
Inferior to the lumbar enlargement, the spinal cord terminates as
a tapering, conical structure called the conus medullaris (KŌ-nus
med-ū-LAR-is; conus = cone), which ends at the level of the interver-
tebral disc between the first and second lumbar vertebrae (L1–L2) in
adults. Arising from the conus medullaris is the filum terminale
(FĪ-lum ter-mi-NAL-ē = terminal filament), an extension of the pia
mater that extends inferiorly, fuses with the arachnoid mater, and
dura mater, and anchors the spinal cord to the coccyx.
Spinal nerves are the paths of communication between the spinal
cord and specific regions of the body. The spinal cord appears to be
segmented because the 31 pairs of spinal nerves emerge at regular
intervals from intervertebral foramina (Figure 13.2). Indeed, each pair
of spinal nerves is said to arise from a spinal segment. Within the spinal
cord there is no obvious segmentation but, for convenience, the naming
of spinal nerves is based on the segment in which they are located.
There are 8 pairs of cervical nerves (represented in Figure 13.2 as C1–C8),
12 pairs of thoracic nerves (T1–T12), 5 pairs of lumbar nerves (L1–L5),
5 pairs of sacral nerves (S1–S5), and 1 pair of coccygeal nerves (Co1).
Two bundles of axons, called roots, connect each spinal nerve to
a segment of the cord by even smaller bundles of axons called rootlets
(see Figure 13.3a). The posterior (dorsal) root and rootlets contain
only sensory axons, which conduct nerve impulses from sensory
receptors in the skin, muscles, and internal organs into the central
nervous system. Each posterior root has a swelling, the posterior
(dorsal) root ganglion, which contains the cell bodies of sensory
neurons. The anterior (ventral) root and rootlets contain axons of
motor neurons, which conduct nerve impulses from the CNS to
eff ectors (muscles and glands).
As spinal nerves branch from the spinal cord, they pass laterally
to exit the vertebral canal through the intervertebral foramina
between adjacent vertebrae. However, because the spinal cord is
shorter than the vertebral column, nerves that arise from the lumbar,,
Q What is the difference between a horn and a column in the spinal cord?
sacral, and coccygeal regions of the spinal cord do not leave the verte-
bral column at the same level they exit the cord. The roots of these
lower spinal nerves angle inferiorly alongside the filum terminale in
the vertebral canal like wisps of hair. Accordingly, the roots of these
nerves are collectively named the cauda equina (KAW-da ē-KWĪ-na),
meaning “horse’s tail” (Figure 13.2).
Internal Anatomy of the Spinal Cord
A transverse section of the spinal cord reveals regions of white matter
that surround an inner core of gray matter (Figure 13.3). The white
matter of the spinal cord consists primarily of bundles of myelinated
axons of neurons. Two grooves penetrate the white matter of the spinal
cord and divide it into right and left sides. The anterior median fissure
is a wide groove on the anterior (ventral) side. The posterior median
sulcus is a narrow furrow on the posterior (dorsal) side. The gray matter
of the spinal cord is shaped like the letter H or a butterfly; it consists of
dendrites and cell bodies of neurons, unmyelinated axons, and neuro-
glia. The gray commissure (KOM-mi-shur) forms the crossbar of the H.
In the center of the gray commissure is a small space called the central
canal; it extends the entire length of the spinal cord and is filled with
cerebrospinal fluid. At its superior end, the central canal is continuous
with the fourth ventricle (a space that contains cerebrospinal fluid) in
the medulla oblongata of the brain. Anterior to the gray commissure is
the anterior (ventral) white commissure, which connects the white
matter of the right and left sides of the spinal cord.
In the gray matter of the spinal cord and brain, clusters of
neuronal cell bodies form functional groups called nuclei. Sensory
nuclei receive input from receptors via sensory neurons, and motor
nuclei provide output to eff ector tissues via motor neurons. The gray
matter on each side of the spinal cord is subdivided into regions
called horns (Figure 13.3). The posterior (dorsal) gray horns con-
tain axons of incoming sensory neurons as well as cell bodies and
axons of interneurons. Recall that cell bodies of sensory neurons are
located in the posterior (dorsal) root ganglion of a spinal nerve. The
anterior (ventral) gray horns contain somatic motor nuclei, which are
clusters of cell bodies of somatic motor neurons that provide nerve
impulses for contraction of skeletal muscles. Between the posterior
and anterior gray horns are the lateral gray horns, which are present
only in thoracic and upper lumbar segments of the spinal cord. The
lateral gray horns contain autonomic motor nuclei, which are clusters
of cell bodies of autonomic motor neurons that regulate the activity
of cardiac muscle, smooth muscle, and glands.
The white matter of the spinal cord, like the gray matter, is
organized into regions. The anterior and posterior gray horns divide
the white matter on each side into three broad areas called columns:
(1) anterior (ventral) white columns, (2) posterior (dorsal) white
columns, and (3) lateral white columns (Figure 13.3). Each column
in turn contains distinct bundles of axons having a common origin
or destination and carrying similar information. These bundles,
which may extend long distances up or down the spinal cord, are
called tracts. Recall that tracts are bundles of axons in the CNS,
whereas nerves are bundles of axons in the PNS. Sensory (ascend-
ing) tracts consist of axons that conduct nerve impulses toward the
brain. Tracts consisting of axons that carry nerve impulses from the
brain are called motor (descending) tracts. Sensory and motor
tracts of the spinal cord are continuous with sensory and motor
tracts in the brain.
The internal organization of the spinal cord allows sensory input
and motor output to be processed by the spinal cord in the following
way (Figure 13.4):
1 Sensory receptors detect a sensory stimulus.
2 Sensory neurons convey this sensory input in the form of nerve
impulses along their axons, which extend from sensory receptors
into the spinal nerve and then into the posterior root. From the
posterior root, axons of sensory neurons may proceed along
three possible paths (see steps 3 , 4 , and 5 ).
3 Axons of sensory neurons may extend into the white matter of the
spinal cord and ascend to the brain as part of a sensory tract.
4 Axons of sensory neurons may enter the posterior gray horn and
synapse with interneurons whose axons extend into the white
matter of the spinal cord and then ascend to the brain as part of a
sensory tract.
5 Axons of sensory neurons may enter the posterior gray horn and
synapse with interneurons that in turn synapse with somatic
motor neurons that are involved in spinal reflex pathways. Spinal
cord reflexes are described in more detail later in this chapter.
6 Motor output from the spinal cord to skeletal muscles involves
somatic motor neurons of the anterior gray horn. Many somatic
motor neurons are regulated by the brain. Axons from higher
brain centers form motor tracts that descend from the brain
into the white matter of the spinal cord. There they synapse
with somatic motor neurons either directly or indirectly by first
synapsing with interneurons that in turn synapse with somatic
motor neurons.
7 When activated, somatic motor neurons convey motor output in
the form of nerve impulses along their axons, which sequentially
pass through the anterior gray horn and anterior root to enter
the spinal nerve. From the spinal nerve, axons of somatic motor
neurons extend to skeletal muscles of the body.
8 Motor output from the spinal cord to cardiac muscle, smooth
muscle, and glands involves autonomic motor neurons of the
lateral gray horn. When activated, autonomic motor neurons
convey motor output in the form of nerve impulses along their
axons, which sequentially pass through the lateral gray horn,
anterior gray horn, and anterior root to enter the spinal nerve.
9 From the spinal nerve, axons of autonomic motor neurons
from the spinal cord synapse with another group of autonomic
motor neurons located in the peripheral nervous system (PNS).
The axons of this second group of autonomic motor neurons in
turn synapse with cardiac muscle, smooth muscle, and glands.
You will learn more about autonomic motor neurons when the
autonomic nervous system is described in Chapter 15.
The various spinal cord segments vary in size, shape, relative
amounts of gray and white matter, and distribution and shape of gray
matter. For example, the amount of gray matter is largest in the
cervical and lumbar segments of the spinal cord because these seg-
ments are responsible for sensory and motor innervation of the limbs.
In addition, more sensory and motor tracts are present in the upper
segments of the spinal cord than in the lower segments. Therefore,
the amount of white matter decreases from cervical to sacral
segments of the spinal cord. There are two major reasons for this




